These are that i want to review about closed fracture that i got from some sources which is written below.
Epidemiology
Treatment
Introduction
- Fracture, the breaking of a part, especially a bone. A break or rupture in a bone.
- A closed fracture is a fracture that does not produce an open wound in the skin.
- A closed fracture occurs when there is bone breakage but no break in the skin. typically bruising and swelling are present at the fracture site.
- A closed fracture is when the bone breaks but there is no puncture or open wound in the skin.
- Called also simple fracture
- Almost all fractures are osteoporotic, in that the risk of fracture increases as bone density decreased.
- Women have a higher risk of fractures than men.
- About 1.5 million osteopororsis-related fractures occur each year. 700,000 vertebral fractures ( U.S)
- In a two-year preiod, 15,293 adults, 7428 males and 7865 females, sustained a fracture.
- Betweem 15-49 years old, males were 2.9 times more likley to sustain a fracture than females (95% CI 2.7 to 3.1)
- Over the age of 60 years, females were 2.3 times more likely to sustain a fracture than males (95% CI 2.1 to 2.4)
Etiology
- A closed fracture is usually caused by an injury to the bone as the result of a fall, accident, or other trauma. Disorders that weaken the bones in the body, such as osteoporosis and cancer, put some people at higher risk for injury.
Mechanisme
- Injury
- Most fractures are caused by sudden and excessive force, which may be direct or indirect.
- With a direct force the bone breaks at the point of impact; the soft tissues also must be damaged.
- Direct force may be : (1) tapping, which causes a tranverse fracture; or (2) Crushing, which causes a comminuted fracture often with extensive soft-tissue damage.
- With an indirect force the bone breaks at a fistance from where the force is applied;soft tissue damage at the fracture site is not inevitavle.
- An indirect force may be ; (1) Twisting cause a spiral fracture; (2) Compression causes a short oblique fracture; (3) Bending results in fracture with a triangular 'butterfly' fragment; (4) Tension tends to break the bone transverly.
- Fatigue or Stress Fracture
- These fractures occur in normal bone which is subject to repeated heavy loading.
- These high loads create minute deformations that initiate the normal process of remodelling.
- When exposure to stress and deformation is repeated and prolonged, resorption occurs faster than replacement and leaves the area liable to fracture.
- Stress fractures are increasingly seen in patients with chronic inflammatory disease who are on treatment with streoids or methotrexate.
- Pathological Fractures
- Fractures may occur even with normal stresses if the bone has been weakend by :
- A change in its structure (e.g in osteoporosis, osteogenesis imperfecta or Paget's disease) or
- Through a lytic lesion (e.g A bone cyst or a metastasis)
Classification of Closed Injuries
- Grade 0
- A simple fracture with little or no soft tissue injury
- Grade 1
- A fracture with superficial abrasion or bruising of the skin and subcutaneous tissue
- Grade 2
- A more severe fracture with deep soft tissue contusion and swelling
- Grade 3
- A severe injury with marked soft tissue damage and a threatened compartment syndrome
Clinical Features
- History
- There is usually a history of injury but the fracture is not always at the site of the injury.
- The patient's age and mechanism of injury are important
- Always enquire about symptoms of associated injuries :
- Pain and swelling elsewhere, numbness or loss of movement, skin pallor or cyanosis, blood in the urine, abdominal pain, difficulty with breathing or transient loss of consiciousness.
- It's important, in preparation for anaesthesia or operation.
- General Signs
- Follow the ABCs
- Look for, and if necessary attend to, Airway obstruction, Breathing problems, Circulatory problems and Cervical spine injury.
- During the secondary survey it will also be necessary to exclude other previously unsuspected injuries and to be alert to any possible predisposing cause
- Local Signs
- Look
- Swelling, bruising and deformity may be obvious, but the skin is not intact.
- Feel
- Gently palpated for localized tenderness.
- The common and characteristic associated injuries should also be felt for, even if the patient doesn't complain of them.
- Vascular and peripheral nerve abnormalitis shoud be tested for both before and after treatment.
- Move
- Crepitus and abnormal movement may be present.
- X-Ray : Rule of Two
- Two views
- A fracture or a dislocation may not be seen on a single X-ray film, at least two views (Anteroposterior & Lateral) must be taken.
- Two joints
- However, is impossible unless the other bone is also broken, or a joint dislocated. The joint above and below the fracture must both the included on the X-ray films.
- Two limbs
- X-ray of the uninjured limb are needed for comparison.
- Two injuries
- Severe force often causes injuries at more than one level.
- Two occasions
- Some fractures are notoriously difficult to detect soon after injury, but another X-ray examination a week or two later may show the lesion.
Treatment
- Consist of manipulation to improve the position of the fragments, followed by splintage to hold them together until they unite; meanwhile joint movement and function must be preserved. Fracture healing is promoted by physiological loading of the bone, so muscle activity and early weighbearing are encouraged.
- These objective are covered by three simple injunction :
A. Reduction
- There are some situations in which reduction is unnecessary : (1) When there is little or no displacement; (2) when displaccement does not matter initially (e.g In fractures of the clavicle) and; (3) when reduction is unlikely to succed (e.g with compression fractures of the vertebrae)
- There are two methods of reduction
- Closed Reduction
- Three-fold manoeuvre : (1) The distal part of the limb is pulled in the line of the bone; (2) As the fragments disengage, they are repositioned (by reversing the original direction of force if this can be deduced) and; (3) Alignment is adjusted in each plane.
- Used for all minimally displaced fractures.
- This avoids direct manipulation of the fracture site by open reduction, which damages the local blood supply and may lead to slower healing times
- Open Reduction
- Indicated : (1) When closed reduction fails, either because of difficulty in controlling the fragments or because of difficulty in controlling the fragments or because soft tissues are interposed between them; (2) When there is a large articular fragment that needs accurate positioning or; (3) For traction (avulsion) fractures in which the fragments are held apart.
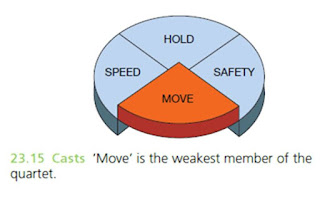
B. Hold Reduction
Methods :
- Continuous Traction
- Cast Splintage
- Functional Bracing
- Using either plaster or one of the lighter thermoplastic materials, to preventing joint stiffness.
- Applied only over the shafts of the bones, leaving the joints free;the cast segments are connected by metal or plastic hinges that allow movement in one plane.
- Used most widely for fractures of the femur or tibia.
- The fracture can be held reasonably well;the joints can be moved; the fracture joints at normal speed; without keeping the patient in hospital and the method is safe.
- Internal Fixation
- Bone fragments may be fixed with screws, a metal plate held by screws.
- Indication
- Fractures that cannot be reduced except by operation
- Fractures that are inherently unstable and prone to redisplace after reduction
- Fractures that unite poorly and slowly
- Pathological fractures
- Multiple fracture.
- External Fixation
- A fracture may be held by transfixing screws or tensioned wires that pass throug the bone above and below the fractures and are attached to an external frame.
- Indication
- Fractures associated with severe soft-tissue damage.
- The soft tissues are too swollen to allow safe surgery.
- Patients with severe multiple injuries, especially if there are bilateral femoral fractures.
- Ununited fractures,
- Infected fractures.
C. Exercise
- More correctly, restore function -not only to the injured parts but also to the patient as a whole.
- Prevention of oedema.
- Elevation.
- Active exercise.
- Assisted movement
- Functional activity.
References
- Apley's System of Orthopaedics and Fractures, Ninth Edition.
- Textbook of Disorder and Injuries of The Musculoskeletal System, R.B. Salter.
- Emedicine.medscape
- Nlm.nih.go
- Web.md
- Illustrated Medical Dictionary, Dorland
Note :
So sorry if there are so many mistakes, please kindly write the suggestion and for the correction.
You're able to rewrite this article, but always noted the references or the sources.
Thanks for reading.















Thank you for your review, it really helps me
BalasHapus